If I have a Mastectomy Do I Need Chemo?

Breast Swollen After Lumpectomy
June 28, 2024
Breast lump for 10 years
August 9, 2024
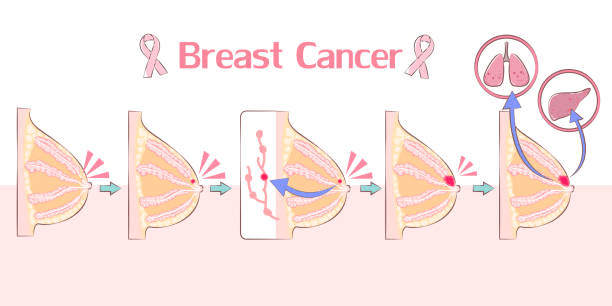
Breast cancer profoundly impacts patients’ lives, both physically and emotionally. A mastectomy, the surgical removal of one or both breasts, is a standard treatment for breast cancer. However, many patients worry about the additional need for chemotherapy after surgery. If I have a mastectomy do I need chemo? According to Dr. Garvit Chitkara, a renowned breast cancer surgeon in Mumbai:
“Each patient’s situation is unique. We perform comprehensive evaluations, including genetic profiling and assessing overall health, to determine the best course of action. This individualized approach allows the doctor to tailor treatment plans to maximize effectiveness and minimize unnecessary side effects.”
Are you wondering, ‘If I have mastectomy, do I need a chemo?’ Please consult a breast cancer specialist to help you make informed decisions about your treatment plan.
So, is chemotherapy compulsory after mastectomy? Let’s delve deeper to find out.
Is Chemotherapy Compulsory After Mastectomy?
Understanding whether chemotherapy is necessary after a mastectomy requires careful evaluation. Dr. Garvit Chitkara, a trusted breast cancer surgeon in Mumbai, says:
“If I have a mastectomy, do I need chemo? Chemotherapy is not compulsory for every patient. The decision is influenced by the type and stage of the cancer, the involvement of lymph nodes, and specific tumor characteristics such as hormone receptor status and HER2 status.
Chemotherapy can help if the cancer is aggressive, has spread to the lymph nodes, or if there is a high risk of recurrence. In some cases, if the cancer is detected early and is localized, surgery alone might be sufficient.”
Oncologists will perform various tests, such as genetic profiling and hormone receptor analysis, to tailor the treatment to your needs. The decision to undergo chemotherapy is made after thoroughly assessing these factors, ensuring the best possible outcome for each patient.
Is the question, ‘If I have mastectomy, do I need a chemo?’ still on your mind? While it’s essential to understand whether chemotherapy is needed, knowing its benefits can help make an informed decision.
Benefits of Chemotherapy After Mastectomy
Chemotherapy after a mastectomy can play a crucial role in the management and treatment of breast cancer. Here are some of the key benefits of chemotherapy:
Eradication of Microscopic Disease:
Chemotherapy helps destroy any cancer cells that may remain after surgery but are too small to be detected, even with scans.
Reduction in Cancer Recurrence:
Chemotherapy reduces the risk of cancer returning both in the same area as the original tumor and elsewhere in the body.
Systemic Therapy:
Since chemotherapy circulates throughout the body, it offers a systemic treatment approach. It can target cancer cells that may have spread beyond the breast and regional lymph nodes.
Increased Survival Rates:

For many patients, particularly those with high-risk breast cancer, chemotherapy can significantly improve long-term survival rates.
Tailored Treatment:
The doctor can tailor chemotherapy regimens based on the individual’s cancer subtype, genetic makeup, and overall health. It allows for personalized treatment plans that are more effective and have fewer side effects.
Adjuvant Therapy:
Chemotherapy is often used as an adjuvant therapy, meaning it is given after surgery to maximize its effectiveness. It’s beneficial in cases where the cancer is aggressive, or other factors increase the likelihood of recurrence.
Equally crucial is understanding the potential risks associated with chemotherapy following mastectomy.
Risks of Chemotherapy After Mastectomy
Chemotherapy after a mastectomy, while beneficial for many, also carries various risks and side effects. If you have a mastectomy do you still need chemo? Here are some of the common risks associated with chemotherapy in this context:
Side Effects:
Common side effects include nausea, vomiting, hair loss, and fatigue.
Damage to Healthy Cells:
Chemotherapy targets rapidly dividing cells, which include not only cancer cells but also other rapidly dividing healthy cells in the body. These may consist of healthy cells in the hair follicles, digestive tract, and bone marrow.
Increased Risk of Infection:
As chemotherapy can reduce white blood cell counts, the body’s ability to fight off infections can significantly weaken, leading to an increased risk of infections.
Neuropathy:
Some chemotherapy drugs can cause peripheral neuropathy, which involves nerve damage. It can lead to symptoms such as pain, burning, tingling, or numbness, especially in the hands and feet.
Cardiotoxicity:
Certain chemotherapy drugs can affect heart health, potentially leading to long-term cardiovascular issues.
Cognitive Effects:
Some patients may experience a phenomenon often called “chemo brain”. This can include memory lapses, trouble concentrating, and other cognitive impairments during and after treatment.
Impact on Fertility:
Chemotherapy can affect fertility in both men and women, sometimes leading to temporary or permanent infertility.
Emotional and Psychological Impact:
The physical effects of chemotherapy can also impact mental health, leading to depression or anxiety.
Long-term Risk of Secondary Cancers:
While rare, some types of chemotherapy can increase the risk of developing a second cancer later in life.
Bone Density Loss:
Some chemotherapy agents can lead to decreased bone density, increasing the risk of fractures.
The potential risks of chemo may make you ask the question – ‘If I have mastectomy, do I need a chemo?’ Each person’s risk profile may vary based on the specific drugs used, the duration of therapy, and their health status.
Engage in a thorough conversation with your healthcare provider. They’ll offer comprehensive insights into the risks and effective strategies for managing any side effects.
Timing is critical for chemotherapy’s effectiveness. But when exactly should you start this treatment after a mastectomy? Let’s explore.
When To Start Chemotherapy After Mastectomy?
The timing of chemotherapy post mastectomy is crucial for its effectiveness. Dr. Garvit Chitkara, a seasoned breast cancer surgeon in Mumbai, advises:
“Chemotherapy typically starts within 4 to6 weeks after surgery. This period allows sufficient time for the surgical site to heal while ensuring that cancer cells are targeted promptly. However, the exact timing may vary based on individual recovery rates and overall health.”

It’s essential to have a detailed discussion with your oncologist to determine the best timeline for starting chemotherapy. They will consider factors such as your body’s healing process, the type of chemotherapy drugs being used, and any other concurrent treatments you might be undergoing.
Conclusion
Deciding whether to undergo chemotherapy after a mastectomy is a complex and highly personalized decision. By understanding the benefits and risks, you can make an informed choice that aligns with your health needs and circumstances. Always consult your oncologist and healthcare team to determine the most appropriate treatment plan.
For comprehensive treatment, consult a breast cancer specialist who can provide personalized guidance and support throughout your journey. Take proactive steps towards your health and well-being by seeking expert advice today.
FAQs
At what stage of breast cancer do you need chemotherapy?
Chemotherapy is typically recommended for breast cancer patients in the advanced stages, if the cancer has spread to the lymph nodes or if it is hormone receptor-negative. Need for chemotherapy is also dependent on the age of the patient.
What type of breast cancer does not require chemo?
Some types of breast cancer, such as early-stage hormone receptor-positive cancers, may not require chemotherapy. However, the decision ultimately depends on tumor size, grade, and genetic markers.
What are the long-term side effects of mastectomy?
While mastectomy can be an effective treatment for breast cancer, it may lead to long-term side effects such as:
- Changes in sensation
- Lymphedema (swelling in the arm)
- Emotional impacts like body image issues and anxiety
Regular follow-up care and support from healthcare professionals can help manage these effects efficiently.
Reference Links:
https://www.moffitt.org/cancers/breast-cancer/faqs/will-i-need-chemotherapy-after-a-total-mastectomy
https://www.mayoclinic.org/tests-procedures/chemotherapy-for-breast-cancer/about/pac-20384931