Living 30 Years with Metastatic Breast Cancer

Pain in Breast One Year After Lumpectomy
December 24, 2024
Nerve Pain After Lymph Node Removal: Causes & Solutions
January 17, 2025
Introduction
Metastatic breast cancer (Stage IV) is often viewed as a terminal diagnosis, but advancements in medicine have shown that long-term survival is achievable. Living 30 years with metastatic breast cancer is not just a testament to modern treatments but also to the resilience of patients.
Dr. Garvit Chitkara, a distinguished breast cancer surgeon in Mumbai, emphasizes:
“Surviving decades with Stage IV breast cancer requires a multifaceted approach, combining treatment advancements, supportive care, and mental fortitude.”
In this blog, we shall explore the journey, challenges, and milestones of living 30 years with Stage IV breast cancer.
Curious if living this long is truly possible? Let’s examine the reality.
Can You Live 30 Years with Metastatic Breast Cancer?
Yes, it’s possible, though rare. Long-term survival often depends on factors such as the biology of the cancer, the patient’s response to treatments, and access to cutting-edge therapies. For instance, some subtypes of breast cancer, such as hormone receptor-positive types, tend to grow slowly and respond well to hormonal treatments, increasing the chances of extended survival.
A global study revealed that approximately 22% of patients with metastatic breast cancer live beyond five years, with a small percentage exceeding 20 or even 30 years.
Dr. Garvit Chitkara, a sought-after doctor for breast surgery in Mumbai, shares:
“Each patient’s journey is unique, and breakthroughs in cancer care have made what seemed impossible a few decades ago a reality today.”
Let’s appreciate how a diagnosis affects this journey.
Living 30 Years with Metastatic Breast Cancer: Understanding Diagnosis
Understanding the diagnosis is the cornerstone of managing metastatic breast cancer for decades. A Stage IV diagnosis means cancer has spread beyond the breast to distant organs such as the bones, liver, or lungs.
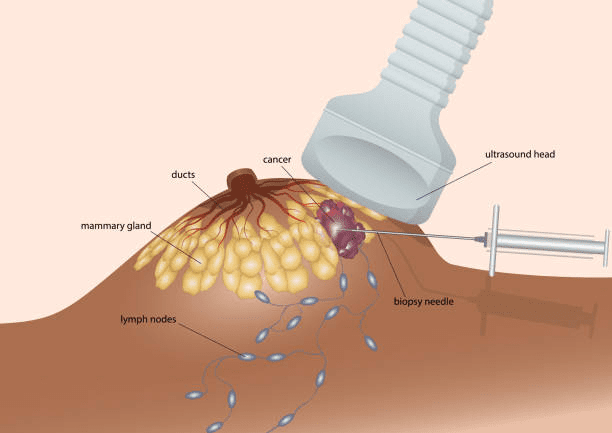
Here are the key diagnostic tools used for metastatic breast cancer:
- Imaging Tests: CT scans, MRI, PET scans, and bone scans to identify the spread of cancer.
- Biopsies: Tissue samples analyzed to confirm the type and progression of cancer.
- Blood Tests: Including tumor marker tests and complete blood counts, to monitor changes in the body.
- Genetic Testing: To assess genetic mutations, such as BRCA1 and BRCA2, which can influence treatment options.
Dr. Garvit Chitkara, an eminent oncoplastic breast surgeon in Mumbai, highlights:
“Advancements in imaging and biopsies allow oncologists to create personalized treatment plans based on the cancer’s characteristics. Routine imaging and blood tests help evaluate treatment success and promptly identify any signs of progression.”
Don’t wait for symptoms to escalate—regular checkups and early interventions could change your life trajectory.
But what about life goals like starting a family? Let’s dive into that.
Can You Have a Baby After Diagnosis?

While metastatic breast cancer treatments like chemotherapy and targeted therapies may affect fertility, advances in reproductive medicine provide options like egg preservation. Patients who achieve stable disease with minimal symptoms might consider pregnancy under strict medical supervision.
Dr. Garvit Chitkara notes:
“Egg preservation is an option to harvest and freeze healthy eggs before cancer treatments begin. It helps safeguard a woman’s ability to conceive in the future, providing a sense of control and hope for starting or expanding a family despite the challenges of metastatic breast cancer. Collaboration between oncologists and fertility specialists is key to ensuring safety and success.”
Now, let’s talk about what survival looks like in terms of life expectancy.
Living 30 Years with Metastatic Breast Cancer: Impact on Life Expectancy
Living 30 years with metastatic breast cancer is extraordinary and depends on continuous advancements in treatment. While the average metastatic breast cancer life expectancy ranges from 2-5 years, some patients defy the odds with modern therapies, improved symptom management, and lifestyle changes.
Long-term survivors often attribute their success to targeted treatments and lifestyle modifications such as maintaining a healthy diet and regular exercise.
Let’s explore the treatments that make this possible.
Treatment Options for Individuals Living 30 Years with Metastatic Breast Cancer
Treatment has evolved significantly, offering options tailored to each patient’s needs:
Hormonal Therapy: Effective for hormone receptor-positive breast cancers.
Targeted Therapy: Drugs like HER2 inhibitors have revolutionized care.
Immunotherapy: Helps the body’s immune system attack cancer cells.
Palliative Care: Focuses on quality of life by managing symptoms and side effects.
Adapting treatments as cancer evolves is the key to surviving decades. Regular discussions with oncologists about clinical trials or emerging therapies are crucial.
Consult a highly knowledgeable breast cancer specialist and explore every option—your treatment plan can evolve just as medicine does.
But what about symptoms that arise over the years? Let’s examine one significant challenge.
Living 30 Years with Metastatic Breast Cancer: Menopausal Symptoms and Their Impact
Treatments for metastatic breast cancer, especially hormone therapies, often induce menopause, leading to symptoms like hot flashes, mood swings, and bone density loss.
Managing these symptoms is essential for long-term quality of life. Options include:
- Non-hormonal medications for hot flashes.
- Bone-strengthening agents to prevent fractures.
- Regular physical activity to improve mood and bone health.
What role does supportive care play in this journey?
Supportive Care for 30 Years with Metastatic Breast Cancer
Supportive care addresses the emotional, psychological, and physical challenges of living with metastatic breast cancer. Long-term survivors often credit their success to the following:
Psychological Support: Counseling and support groups.
Nutritional Guidance: Specialized diets to maintain energy and immunity.
Pain Management: Medications and therapies like acupuncture.
Dr. Garvit Chitkara, a skilled professional in axillary surgery, emphasizes:
“Supportive care is not an add-on; it’s an integral part of comprehensive cancer management. By addressing mental well-being, physical symptoms, and dietary needs, we create a holistic approach that enhances quality and length of life.”
When should you consult your doctor? Let’s find out.
When to Consult a Doctor During 30 Years with Metastatic Breast Cancer
Ongoing communication with a healthcare provider is critical. Patients should immediately consult a doctor if they experience new symptoms such as persistent pain, swelling, or unexplained weight loss. These could signal disease progression or treatment side effects.
Don’t ignore red flags—prompt action could make all the difference.
Conclusion
Living 30 years with metastatic breast cancer is no small feat, requiring a mix of advanced treatments, personalized care, and resilience. While every patient’s journey is unique, the right support system and proactive health management can significantly improve survival and quality of life.
Have more questions? Let’s address them below.
Frequently Asked Questions:
1. Which celebrities are living with metastatic breast cancer? still have pain after a lumpectomy?
Several public figures, including Shannen Doherty, have openly shared their metastatic breast cancer journeys, inspiring many with their resilience and advocacy.
2. Are there people living 20 years with metastatic breast cancer?
Yes, many long-term survivors have lived 20 or more years, particularly with hormone receptor-positive cancers managed through ongoing treatment.
3. What are the red flag signs of metastatic breast cancer?
Signs include unexplained pain, lumps in unusual places, persistent fatigue, or changes in appetite. Always consult a doctor if you notice these symptoms.
4. What is the metastatic breast cancer survival rate?
The 5-year survival rate is about 22%, but advancements in treatment have significantly increased the number of long-term survivors.
5. What lifestyle changes improve long-term survival?
A balanced diet, regular exercise, stress management, and adherence to treatment plans contribute to better outcomes and quality of life.
6. Can metastatic breast cancer go into remission?
Yes, while rare, periods of remission are possible with effective treatments and close monitoring.
7. How does stress impact metastatic breast cancer?
Chronic stress can weaken the immune system, potentially affecting treatment efficacy. Stress management techniques like yoga or meditation can be beneficial.
Reference links:
https://www.breastcancer.org/types/metastatic/life-with-metastatic/advice-for-newly-diagnosed
https://my.clevelandclinic.org/health/diseases/21497-metastatic-breast-cancer
Disclaimer: The information shared in this content is for educational purposes only and not for promotional use.

