Menopause marks a significant transition in a woman’s life, bringing about hormonal changes that can affect various aspects of health, including breast tissue. As estrogen and progesterone levels decline, many women notice changes in their breasts—some experience increased tenderness, lumpiness, or cyst formation, even after menopause.

Dr. Garvit Chitkara, a trusted Breast Cancer Surgeon in Mumbai, says:
“Menopause is often thought to bring an end to breast-related discomfort, but for some women, fibrocystic breast changes persist. These changes can increase lumpiness and sensitivity, often causing unnecessary alarm. While fibrocystic breasts after menopause are usually benign, it’s crucial to differentiate them from other breast conditions through proper evaluation.”
Wondering how survival rates apply to your situation? Every case is unique, and personalized guidance can make all the difference. Get expert insights on your diagnosis and treatment options today!
So, what exactly causes fibrocystic breasts after menopause, and should you be concerned? Let’s explore.
Fibrocystic Breasts After Menopause – Causes
Although fibrocystic breast changes are more common in premenopausal women, studies indicate that up to 15-20% of postmenopausal women still experience fibrocystic breast disease, especially those on hormone replacement therapy (HRT).
Some of the primary causes include:

Hormone Replacement Therapy (HRT) – Many women take HRT to manage menopausal symptoms, but the additional estrogen can stimulate breast tissue, leading to cystic changes.
Residual Hormonal Activity – Even without HRT, the body continues to produce small amounts of estrogen, which can impact breast tissue.
Breast Tissue Composition – Women with naturally dense breasts are more prone to persistent fibrocystic changes, regardless of menopause.
Caffeine and Diet – Excess caffeine, high-fat diets, and processed foods have been linked to increased breast cyst formation.
Dr. Garvit Chitkara, a renowned Oncoplastic Breast surgeon in Mumbai, adds:
“Although menopause reduces hormone fluctuations, some factors can still contribute to fibrocystic breast changes. Residual estrogen activity, certain medications, and lifestyle factors can all play a role. Understanding these triggers helps women manage their breast health effectively and minimize discomfort.”
So, how can you tell if your breast changes are harmless or require medical attention? Let’s break it down.
Diagnosis and Monitoring
Recognizing the symptoms and seeking proper evaluation is key. Fibrocystic breast changes often cause:
Lumpiness or nodularity – The breast tissue may feel uneven or rope-like.
Tenderness or pain – This can range from mild discomfort to noticeable pain.
Cyst formation – Fluid-filled sacs may develop and vary in size over time.
Diagnosis:
Clinical Breast Examination (CBE) – A physical exam by a doctor to assess the lumpiness and texture of the breasts.
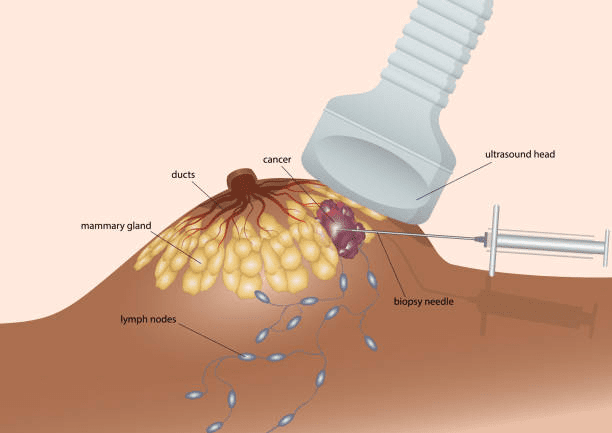
Ultrasound or Mammogram – Imaging tests help distinguish cystic changes from solid lumps.
Fine Needle Aspiration (FNA) or Biopsy – If a lump appears unusual, a sample may be taken for further analysis.
Experiencing persistent breast tenderness or lumpiness after menopause? Don’t ignore these changes—consult a specialist to ensure your breast health is on the right track!
Managing fibrocystic breasts doesn’t have to be complicated. Here’s what you need to know about effective treatment options.
Fibrocystic Breasts After Menopause – Treatment Options
While fibrocystic breast changes don’t require aggressive treatment, various options help manage symptoms:
Pain Management – Over-the-counter pain relievers like ibuprofen can ease discomfort.
Lifestyle Modifications – Reducing caffeine and maintaining a balanced diet can help.
Hormone Therapy Adjustments – If HRT is causing symptoms, adjusting the dosage may be beneficial.
Needle Aspiration – If cysts are large and painful, draining the fluid can provide relief.

Want to reduce discomfort and maintain breast health after menopause? These simple yet effective lifestyle adjustments can help.
Prevention and Lifestyle Tips
Although you cannot always prevent fibrocystic breasts after menopause, certain habits can reduce symptoms:
- Studies suggest reducing caffeine intake and high-fat foods can alleviate symptoms.
- Maintain a healthy weight, as obesity can increase estrogen levels, impacting breast tissue.
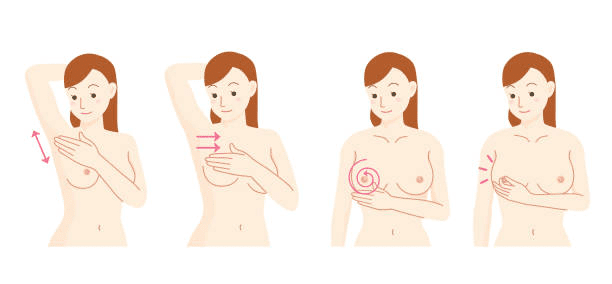
- Regular breast self-exams help in the early detection of abnormalities.
- Proper hydration and a diet rich in fruits and vegetables support overall breast health.
But does having fibrocystic breasts increase cancer risk?
Risk of Breast Cancer with Fibrocystic Breasts After Menopause
One of the most common concerns among women with fibrocystic breasts after menopause is whether they are at a higher risk of breast cancer. Research shows that while fibrocystic breast disease itself is not cancerous, certain atypical changes may slightly increase the risk.
Globally, breast cancer affects over 2.3 million women annually, with postmenopausal women being at higher risk. If fibrocystic changes are accompanied by atypical hyperplasia (abnormal cell growth), the lifetime risk of developing breast cancer may be 3-5 times higher than average.
Dr. Garvit Chitkara, a highly sought after Breast cancer surgeon, advises:
“Although fibrocystic breasts are generally benign, some cases involve cellular changes that warrant closer monitoring. Regular check-ups, imaging, and a proactive approach to breast health can ensure early detection of any potential risks. The good news is that with advancements in breast imaging, we can accurately differentiate benign from concerning changes, giving women greater peace of mind.”
Worried about the risk of breast cancer with fibrocystic breasts? Early detection and regular check-ups can make all the difference. Take charge of your breast health now!
Conclusion
Globally, the average age of menopause is around 51 years, while in India, it occurs earlier, typically between 46 and 49 years. Menopause brings about profound changes in a woman’s body, and breast health is no exception. While many women assume that hormonal shifts will eliminate breast discomfort, conditions like fibrocystic breasts after menopause can persist. However, with proper awareness, lifestyle adjustments, and routine monitoring, women can manage these changes effectively.
Dr. Garvit Chitkara, a prominent breast oncosurgeon in Mumbai, concludes:
“Your breast health matters at every stage of life. If you’re experiencing persistent discomfort or changes in breast tissue, don’t hesitate to seek medical guidance. With the right approach, you can maintain good breast health and overall well-being well beyond menopause.”
Still have questions about fibrocystic breasts after menopause? Here are some of the most common concerns answered.
Frequently Asked Questions
1. Can fibrocystic breast changes occur after menopause?
Yes, though less common, some women continue to experience cystic breasts after menopause, particularly those on hormone replacement therapy (HRT). The hormonal influence on breast tissue may still persist.
2. How can I tell the difference between a fibrocystic lump and breast cancer?
Fibrocystic lumps tend to be soft, movable, and often fluctuate in size, while cancerous lumps are typically hard, irregular, and fixed in place. However, any new lump should always be evaluated by a specialist.
3. Will reducing caffeine help with fibrocystic breast discomfort?
Yes, studies suggest that cutting down on caffeine (found in coffee, tea, and chocolate) can help reduce breast tenderness and cyst formation in some women.
4. Should I stop taking HRT if I have fibrocystic breasts?
Not necessarily. If HRT is causing discomfort, your doctor may recommend adjusting the dosage rather than stopping completely. Each case is unique, so consultation is essential.
5. How often should postmenopausal women with fibrocystic breasts get screened?
Women should continue annual mammograms and clinical breast exams. If you have additional risk factors, your doctor may recommend more frequent imaging such as ultrasound or MRI.
Not sure if your breast changes are normal or a cause for concern? A professional evaluation can provide clarity and peace of mind. Schedule a consultation today!
Reference Links:
https://www.mayoclinic.org/diseases-conditions/fibrocystic-breasts/symptoms-causes/syc-20350438
https://pubmed.ncbi.nlm.nih.gov/37073209
Disclaimer: The information shared in this content is for educational purposes only and not for promotional use.

