Did you know? Each year, over 2.3 million women are diagnosed with breast cancer globally, and a large proportion undergo mastectomy as a part of their treatment journey. While this life-saving surgery is critical in combating cancer, it also brings with it a lesser-known yet significant side effect—nerve regeneration pain after mastectomy.
This form of discomfort is not just “in your head”—it’s a real, biological process that affects thousands of women post-surgery. Understanding this pain and knowing how to manage it effectively is crucial for a full recovery and improved quality of life.
Dr. Garvit Chitkara, a renowned breast oncology surgeon in Mumbai, emphasizes the importance of proactive communication and informed recovery. “Awareness is a patient’s first line of defense. Recognizing symptoms early can lead to better management of nerve pain and reduce long-term complications.”
This blog explores what happens during surgery, why nerve pain occurs, and what you can do about it.
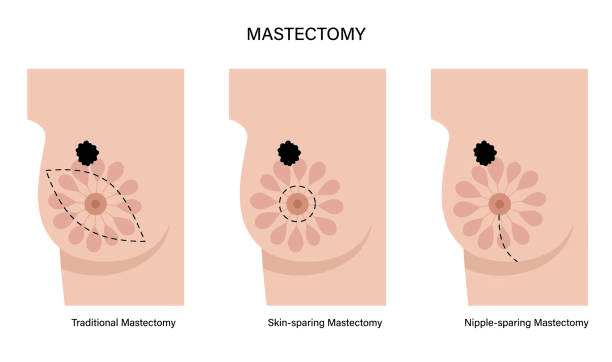
What Happens to Nerves During a Mastectomy?
A mastectomy involves the surgical removal of breast tissue, sometimes including lymph nodes and chest wall muscles depending on the cancer’s stage. In doing so, several sensory nerves in the chest wall and underarm area can be severed or damaged, especially the intercostobrachial nerve, which plays a key role in sensation.
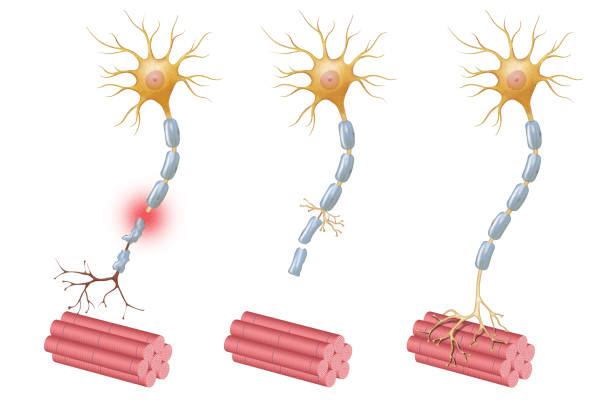
When these nerves are cut, the body begins the natural process of nerve regeneration—an attempt to reconnect disrupted nerve endings. Unfortunately, this healing is rarely smooth and can often trigger sharp, burning, or tingling sensations.
Ever felt pins and needles or shooting pain months after surgery? You’re not alone.
Understanding Nerve Regeneration Pain After Mastectomy
Nerve regeneration pain after mastectomy is a neuropathic pain—originating from the nerves themselves, not an external source. It’s caused by the regrowth of nerve fibers attempting to reconnect and regain function. However, as they grow, these fibers can form neuromas—tangled nerve bundles that are overly sensitive and painful to touch.
Key facts about nerve disruption during mastectomy:
Nerve regeneration begins weeks after surgery.
Damaged nerves may misfire during healing, causing pain.
Some women experience phantom breast pain—sensation in the absent breast.
This is where nerve regeneration pain steps in. Understanding its nature helps reduce fear and enables more informed discussions with your medical team.
Struggling with unexplained chest discomfort post-mastectomy? Don’t ignore it. Learn how to differentiate healing pain from complications.
Quick Facts
Studies show that 20-30% of women experience chronic post-mastectomy pain, often attributed to nerve regeneration. While it’s a part of healing, unmanaged pain can significantly impact your daily life, sleep, and emotional well-being.
Identifying Nerve Pain vs. Concerning Symptoms
It’s essential to differentiate between normal healing and red-flag symptoms that require urgent attention. While nerve regeneration pain is uncomfortable, it’s usually predictable and follows a certain pattern. On the other hand, signs like redness, swelling, or persistent fever might indicate infection or other surgical complications.

Burning or stabbing pain in the chest wall or underarm
Hypersensitivity to touch or clothing
Electric-shock-like sensations
Numbness that gradually transitions into pain
Comes and goes in waves
Typically worsens with stress or cold weather
This pain can begin weeks or even months after surgery and may persist without proper intervention.
Red-flag symptoms:
- Persistent, deep-seated pain not improving over time
- Swelling or inflammation near the surgical site
- High fever or pus discharge
- Sudden hard lumps in the chest wall
Dr. Garvit Chitkara advises, “Don’t dismiss lingering pain as something you have to live with. Keeping a pain diary can help track symptoms, identify patterns, and facilitate clearer communication with your breast surgeon. The sooner we intervene, the better the outcomes—both physically and emotionally.”
Concerned about a breast indentation or related symptoms? Get a diagnostic evaluation from an expert breast specialist. Schedule a consultation today.
Management and Treatment Options for Nerve Pain After Mastectomy
1. Medications
Neuropathic pain relievers
NSAIDs to reduce inflammation
Topical patches for localized relief
2. Physical Therapy
Gentle exercises guided by a specialist can prevent nerve entrapment and improve blood circulation, reducing pain intensity over time.
3. Desensitization Techniques
Rubbing soft materials on the area or light massage can retrain the nerves and reduce hypersensitivity.
4. Nerve Blocks
In resistant cases, nerve block injections can temporarily numb the area, providing both diagnostic and therapeutic value.
5. Mind-Body Techniques
Meditation
Guided imagery
Cognitive Behavioral Therapy (CBT)
These can help you cope with chronic pain and its emotional toll.
Managing nerve pain isn’t a one-size-fits-all solution. Consult a breast specialist to understand the best combination for your body’s healing.
Wondering when your pain is “too much” or “not normal”?
When to Talk to Your Breast Surgeon
Post-mastectomy recovery varies from person to person. However, if pain persists beyond 3 months and impacts your quality of life, it’s time to speak with your breast cancer surgeon or pain management specialist.
Schedule a follow-up if you experience:
Pain worsening over time
Emotional distress or anxiety related to pain
Disruption in sleep or daily activities
Unresponsive symptoms despite medication
Dr. Garvit Chitkara, a prominent breast cancer surgeon in Mumbai, emphasizes, “Your post-operative care is just as important as your surgery. Persistent nerve pain is not a sign of weakness—it’s a signal that your body needs attention. Early consultation allows for timely adjustments in treatment, helping you return to your normal routine sooner.”
Conclusion
Nerve regeneration pain after mastectomy is a real, manageable aspect of recovery—not something to suffer in silence. From understanding its cause to exploring various treatment options, being proactive is key. This pain signifies your body’s effort to heal and reconnect, and with proper guidance, you can navigate it confidently.
Dr. Garvit Chitkara’s approach combines surgical precision with long-term recovery planning, ensuring patients don’t just survive breast cancer but thrive afterward.
Pain shouldn’t define your recovery. Empower yourself withexpert insights and take charge of your post-mastectomy healing.
Frequently Asked Questions
Q1: How long does nerve regeneration pain last after mastectomy?
A: It varies. Some patients experience pain for a few weeks, while others may continue for several months. Chronic pain beyond 3-6 months may require intervention.
Q2: Is nerve regeneration pain dangerous?
A: No, it’s usually a natural part of healing. However, it can be distressing if not managed. Always differentiate it from signs of infection or recurrence.
Q3: Can physical therapy help with nerve pain?
A: Yes. A physiotherapist can guide gentle exercises that reduce nerve tension and promote circulation, easing discomfort over time.
Q4: Is it common to feel pain in the absent breast?
A: Yes. This is known as phantom breast pain and is related to the nervous system continuing to send signals from the amputated area.
Q5: Should I avoid using my arm on the side of the surgery?
A: Initially, rest is important. But with guidance, gentle movement is encouraged to prevent stiffness and support nerve recovery.
References:
https://www.hopkinsmedicine.org/health/conditions-and-diseases/breast-cancer/mastectomy
https://www.cancer.org/cancer/managing-cancer/side-effects/pain/post-mastectomy-pain-syndrome.html
Disclaimer: The information shared in this content is for educational purposes only and not for promotional use.

